AMaT podcast
The clinical audit and improvement podcast
We bring together experts to talk about a range of topics for the benefit of everyone involved in clinical audit and improvement projects across healthcare.
Our latest guests
Isabel Dighero
Isabel Dighero is a core surgical trainee at Epsom and St Helier University Hospitals NHS Trust.
Molly Nichols
Molly Nichols is a core surgical trainee at Barts Heath NHS Trust.
Improving patient care in Urgent Treatment Centres
Dom Conlon: Hello and welcome to the Clinical Audit and Improvement podcast from AMaT. The audit, management and tracking tool, which is developed in partnership with our users. So my name is Dom Conlon. And in this episode we're going to be talking about improving patient care in urgent treatment centers.
And with me to discuss the subject are three guests. We've got Vicky Barsby, Cassandra Dye and Neil Jones, and they're all from Derbyshire Community Health Services.
Vicky first is an improvement, innovation and effectiveness facilitator. She started her NHS career as the IT Clinical Systems Training Lead and caught the bug for audit when she undertook some service improvement projects. Prior to that she was a teacher specialising in supporting children with additional needs, and Vicky continues to support staff in her current role so that they can go on supporting patients.
And then we have Cassandra and Cassandra is a data analyst and sheer practitioner who started in the NHS as an admin apprentice way back in 2010. After an organisational restructure, Cassandra became a quality compliance officer before beginning training for her current role. She's a black belt in Lean Six Sigma and works within the Improvement, Innovation and Effectiveness team.
And finally we've got Neil. Neil's a service lead for the North Urgent Treatment centers. He's had 27 years' experience as a qualified nurse within urgent and emergency care, including out of hours. And he's also a resuscitation council advanced life support provider. So loads of experience as usual on the podcast today. And thank you, all of you for joining me and giving up your time to discuss this.
So, Neil, I think we're going to have to go to you first because you kind of started this whole thing off. You're the service lead for the urgent treatment centers. So could you just give us a kind of picture, an overview of what was going on that led to this improvement in care.
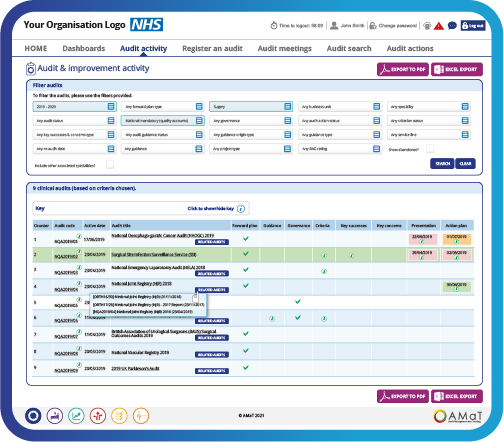
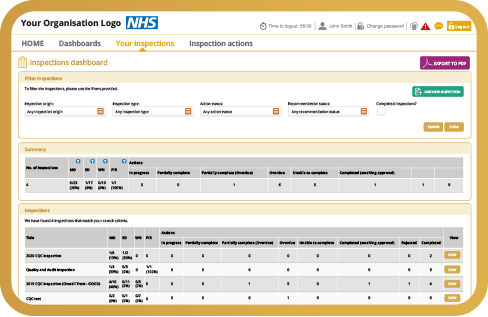
Neil Jones: Absolutely. So within our organization, we have four urgent treatment centers spread across the county. And back in the day when we were undertaking audits, we had lots and lots of different audits on different bits of paper, different spreadsheets. And the NHS was provided in little pockets of primary care trusts. So there were headed paper for one, headed paper for another, and never the twain shall meet. And it was really, really difficult to collate the information we wanted across all four units. And funnily enough, recently, whilst clearing out a filing cabinet, we discovered a whole ream of papers which were our old fashioned peer review audits from 20 pre, going onto electronic patient records and electronic systems such as AMaT. And what my colleagues from the innovation team, with AMaT that was being developed and implemented within our organization, said, we've got this great tool, you might like to use it. And we went, okay, that sounds really good. We've got lots of papers. We can't amalgamate things very well. We can't see clear themes. It's very, very difficult to pull together what the information that we would like, in order to pay to improve patient care. But to showcase what we're doing is right, but equally showcase where we could make improvements. And it was really difficult to pull all that together until everything went onto AMaT. And that's been revolutionary and that's where we are now.
Dom Conlon: So this must have been kind of music to your ears. Vicky and Cassie, does one of you want to kind of take up the story from there? I mean, what was your response to this?
Cassandra Dye: I was the analyst on the ground at the time. Actually, when Neil had come to the team, I'd just gotten back from maternity leave, and it was my first big project. Oh, yeah. So the UTC's have decided they want to put their entire suite of audits on AMaT. Can you sort that out? And we started off, was it the peer review?
Neil Jones: It was. it was the peer review audits and x ray audits to start with, wasn't it? the first peer.
Cassandra Dye: Review and the x ray quite close together. And everything started snowballing and sort of from my point of view, everyone was excited and they were keen and it was like, oh, can we make it do this for us? Can we make it do that? And it just snowballed. It was an excellent project to come back to actually.
Vicky Barsby: But I think it even sort of snowballed to the Trust as well, because we've got things like our hand hygiene and all our IPC audits onto AMaT as well. So it wasn't only service specific ones to the UTC's in Neil's teams, it went sort of Trust wide as well. So yeah, we use Neil as a shining beacon of how it should be done.
Dom Conlon: Or a guinea pig depending on your...
Neil Jones: Guinea.
Dom Conlon: Pig. So because Derbyshire is quite a spread out kind of Trust, isn't it? Derbyshire community, from what I remember from discussing with other members of the team. So what kind of challenges were involved in this?
Neil Jones: I think probably the first thing was, sort of decide seeing the capabilities of AMaT from our perspective in the clinical service. So we sort of know what we want. We've got all these different audits on lots and lots of bits of paper. We want to be able to look at those details, look at the outcomes of those audits. What outputs can we then take from that? Will this system be able to support us in that? Just a couple of years before AMaT, we'd moved from paper patient records to electronic patient records. So that was a big hike for our service and lots of other services in the organization. So initially there was also some trepidation in terms of, oh, it's another electronic system. Will this work for our service or not? So, a lot of our stalwart staff, shall we say, were, you know, arms crossed. We like our pen and paper. We can physically see it. That's great for that part of the service. Whereas the rest of the service, who might learn something from that bit of paper that that person is holding on to wasn't there. So I think probably for us on a clinical side, it was will this work? How will this help us improve what we're delivering to patients?
Vicky Barsby: I think as well, it's also logistic challenges, because as a community Trust, we are spread out across a massive patch if you like. So it's not as easy as just sort of popping down the corridor to Neil and say, oh, just what do you think about this? It was a lot more about deliberate communications and trying to get together. Well, at the time it was sort of in Covid as well. So you've also got that challenge on top of it as well. So it did make it difficult, but it's not something that we're, it's not new to our Trust. We know the challenges of trying to meet up and communicate different things across a wide community patch.
Dom Conlon: So that must be, so we've had this kind of touched upon in previous episodes about the impact of Covid and how, as difficult as that time was, it also enabled new technologies like Teams to come in. And so like you're saying, you can't pop down the corridor, but did it help at all? having Teams suddenly being accessible to everybody across the whole Trust and things like that?
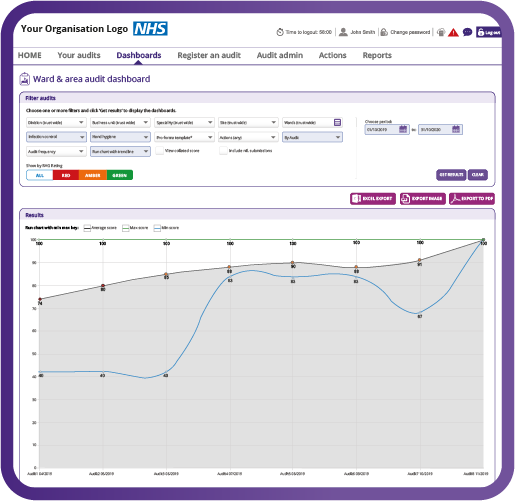
Neil Jones: Certainly from our perspective, yes. Because we were able to then link our four units together with one system to be able to go, okay, so our hand hygiene audit for example overall is this. Oh, and then we can break it down into individual units as well. Can we see themes and trends with the peer review. So in the north of the county, that has a completely different population to the south of the county, where their similarities were, they're completely different, different differences in the results. But equally, are the staff interpreting the audits that they're undertaking same or different? Oh, that was that.
Cassandra Dye: You've just sparked something there, Neil, that interpreting audit questions in the same way, there was a real challenge. made easier by the likes of Microsoft Teams coming in, that we could get people from all four UTCs, and go through all the audit questions to make sure that everyone was understanding it and reading it in the same way. So one of the parts in my role as an analyst is the question you are asking. Will you get the answers you anticipate? Are you asking the right question for what you're expecting out of it? And it was certainly very interesting to have all four UTCs come together and be like, well this is what we think this means, and then try and rephrase the questions to work correctly for what the actual ask was a bit.
Dom Conlon: Yeah. No, no. That's good. That's the stuff. So what kind of audits were being redesigned? What were you, did you start off with just one? or did you go no, we'll do everything all at once.
Neil Jones: We started with one then sort of two quite quickly together. So we started off with a peer review audit. Then we moved on to the x-ray audit, which was a complete and utter game changer. It was brilliant. Still is. And then once we, I think once the clinical side realised the capabilities of having everything in one suite, that's when we said to the guys, please, could we look at equally, what Cassie and Vicky were able to do is say, as Vicky has already mentioned, if there's a Trust audit that we're part of might already be on our map. Let's look at those as well. So we had the service specific and we had the Trust specific ones as well, that we could then bring together in one place. So it evolved over a period of time. But I think because we've we learnt lessons quite quickly, as in, oh this is good. There's lots of capabilities here. It was then easier to onboard all the other audits. It felt more comfortable doing it that way. And if we learned something from one audit we could then implement it on another one, potentially in terms of how it was displayed. As Cassie said, the results that we potentially were expecting, how questions were asked, that sort of thing, I think.
Vicky Barsby: It's that visibility as well increased because everyone could come to AMaT to see what else was happening around the Trust, instead of having to share those bits of paper that Neil mentioned before.
Dom Conlon: You mentioned the x-ray, you Neil, your eyes lit up at the mention of the x-ray. Tell me something about that then. That sounds like an interesting area to explore. Because it sounds really positive that you learned things from it and developed it.
Neil Jones: So one of our key governance loops that we like to close, is when a patient has attended and has a clinical assessment. A part of that clinical assessment is deemed an x-ray is required. The patient will go for an x-ray that will be interpreted by the radiographer very briefly, to decide if there's something that they can physically see immediately to then alert the clinician in the UTC, the UTC clinician will do exactly the same. They'll look at that x-ray, excuse me, they'll interpret it, based on their clinical findings from the patient with the x-ray, to support, to come to a diagnosis and then to close that loop. The x-rays are then reported on either by a consultant orthopaedic surgeon or a reporting radiographer. As part of that governance process, and closing the loop, we then audit the number of x-rays that have been carried out, the number of x rays that we anticipated would be positive so that there's something on there, potentially a fracture or a foreign body, for example. And those that potentially were negative. And again, back down to paper, we had different units doing different things. So some people were doing it on the computer on an Excel spreadsheet. Some people were writing it down on a bit of paper in a folder that was collecting dust on a shelf, that came out once a week for somebody to do the x-ray audit. And it was very difficult to collate everything in terms of the x-ray audit going straight onto AMaT.
Neil Jones: It answered the questions that we wanted. Answering it pulled all four units together. We can see themes and trends. So nationally the Royal College's expect across the NHS in the UK, that any services that are undertaking x-rays for undifferentiated diagnosis. So, anybody who walks in with an injury for example, roughly you should see 50 over 50. So 50% positive, 50% negative because we're hoping to rule in the 50% positive. And that's something that we couldn't readily share outside our organization, because everything was on paper, on different bits of spreadsheets, and never the twain shall meet. Bringing that into AMaT, we're now able to just click onto our map, look at our x-ray audit, look at exactly where we are in terms of 50% higher or lower. We can break it down to individual clinicians. We can break it down by unit. That data is then supplied nationally if and when it's required. And it's also supplied internally as part of our quality always process. So for me, and a lot of my colleagues, the x-ray audit was the game changer that sort of opened our eyes. We saw the wood for the trees at that moment. You know, that light bulb moment where everybody goes, ah, this is going to be really good for other audits, isn't it? If we can get this level of information quickly, centrally. It's a game changer.
Dom Conlon: An x-ray for the x-ray. Excellent. Okay.
Neil Jones: That's right.
Dom Conlon: So Cassie and Vicky. So the data coming in, this must have been again, music to your ears. So what support did you give to Neil and to the rest of the team?
Neil Jones: And still do.
Dom Conlon: And still do? Yes. Of course.
Dom Conlon: Sorry.
Cassandra Dye: Neil's got me on speed dial. To be fair, it started off as quite hand-holding. It was going through the questions. It was are they, are you asking the right questions? That's going to give you the right information. Falling out. It was being able to split things out so that we can do the UTCs as a whole, or do each of the individual UTCs so everyone can see their piece of the puzzle. I've done some support with how to pull the data off and put it into an Excel dashboard that I've created, to give them that real look into what is being said. And then created an instruction document and handed it over.
Cassandra Dye: And they haven't broken it yet?
Neil Jones: Not yet.
Dom Conlon: A challenge has just been extended, I fear. What about training? Was any training necessary? For, say, for everybody else, for people using it? Or did you just kind of all just take to it?
Cassandra Dye: Offered some training, certainly at the start. I think you've done a lot of cascading down yourself with the team, haven't you, Neil? And then I think we sort of stick our hat in once a year, like the UTC away days and support with the wider team.
Dom Conlon: Or when I've got...
Neil Jones: You on speed dial.
Dom Conlon: Yeah.
Vicky Barsby: So we. So Cassie and I and another one of our team members, we recently went to the UTC away days. Neil invited us along to go and have a bit of a section about audits, which isn't as exciting as it sounds.
Cassandra Dye: Proper sexy.
Vicky Barsby: But we do make it. We do make audits sexy. But it was actually a really nice opportunity to speak to staff. So obviously we mainly liaise with Neil and the other UTC managers, but actually getting to talk to staff about the impacts of the audits was really exciting. And it did go to, at one point, a slightly uncomfortable conversation because I sort of said. I went off script and I said, what do you actually think about audits? Do you see the point of them? And they were very honest, very polite and honest, but they sort of said, like, sometimes we don't. We see it as a tick box exercise, which I think is typically what audit feels like sometimes. But that was sort of our flash then of actually, are we sharing the results of the audits well enough? Like I think sort of Neil and the guys, they share them with the staff in possibly hidden ways. So we sort of came up with ideas that they could be shared in more obvious ways and more ways that would have an impact on what staff do day to day as well. So and that was a real nice turning point. It wasn't necessarily training, but it was that engagement side of things that really opened it up to everyone even further.
Cassandra Dye: Argumentatively or Argumentatively. The hardest part is the engagement bit.
Vicky Barsby: Yes, definitely. Definitely trying to get people. I think all the staff at the UTC were on board. They did the audits, they were happy with doing the audits. It's just getting to see that impact and the reason why we're doing the audits and get them really, really engaged, which I think yeah, we're there now.
Dom Conlon: That's excellent. I mean, the transparency and visibility of these things you do want to know what's the point of it. So what of it all. And if you can't see that then yeah, it's hard to engage fully. And you mentioned that resistance right at the beginning. You know we we've always done this on paper. This is the way it's worked and it's worked so far. Which is true, which is great. So what was then looking back, the response presumably that resistance melted away. And is there more, can people now see the benefits of doing it this way?
Neil Jones: Certainly. I think that resistance began to melt. Probably took a while for, for some people. Yeah, definitely. We have a lot of staff now doing, advanced clinical courses at university. And what we found is, when they're undertaking their studies at university level, they're looking for information to support writing assignments and things, and they now know that they can go to AMaT if there's a subject that they're writing about that we deal with on AMaT, they can go to that and get the information that they need to support their academic writing as well. So there's certainly a cohort of engaged staff already, that absolutely love it. And I think that Vicky said the barriers with the others have broken down, particularly those who are actively engaged in undertaking the audits. Because they go to AMaT, they can see it. And one of the things that we've learned from the away days last year, in terms of sharing it, sharing the results completely out there in the teams is by putting results of certain audits in our bi-monthly newsletter, which goes by email to every single member of staff. So that was an action that we took from inviting the guys to come to the away days. So that was absolutely brilliant. Fab.
Dom Conlon: That sounds fantastic lessons. Glad to have learned some lessons from all this. It sounds a really kind of involved process and full of challenges. So what kind of lessons have been learned from both, from you and from Neil and from you Cassie and Vicky?
Cassandra Dye: Don't do it. It's a lot of work.
Dom Conlon: And thank you for joining us.
Vicky Barsby: I think when we had a bit of a conversation about this, it was sort of with hindsight, were we sometimes too concerned with the testing and to where it sort of take that final step and let's just launch it and let's go. So I think we.
Cassandra Dye: Yeah, we were really nervous because it was quite early in us using AMaT as well, and we were really nervous about using ward area at the time. Some of it being because once it was launched, you then, it felt like you couldn't make changes until the next audit cycle. And that was quite daunting from an us point of view in our team. It felt like we had to get it right first time, when maybe we didn't know.
Vicky Barsby: We've definitely learned from that now. And sometimes we leap before we should leap sort of thing. So yeah. Yeah, that's definitely changed now.
Neil Jones: I think it was sort of mentioning earlier we've learnt about the language of questions as the audits have gone along. So, the one of the latest audits to be uploaded onto AMaT is the effective documentation review audit. And we spent quite a proportion of our time thinking about the questions in this one. So we knew what we wanted to ask. We knew how we can launch it. As Vicky said, we weren't as scared or as worried about launching it. But there was a lot of looking at the ingredients. How can we get these ingredients right so that when it's baked, everybody understands how it's been baked? That was the easiest sort of way of we were really, really engaged in that. And I think that was probably the lesson. There was not to focus on it too much either, because we could have gone round in circles 20 times. To say what we wanted to say, but it was about that. Okay, so we've thought about this 2 or 3 times now. This is we need to make this as clear as possible. This is what we think it is. Okay. Let's move on.
Cassandra Dye: Yeah I think there's also with your baking or cooking analogy there, too many cooks spoil the broth. Yes. Having too many people in the room made us very unproductive. But getting the right people in the room does absolute wonders.
Dom Conlon: So would you do anything? Would you look back and do anything differently? I mean, are you doing this kind of process for other areas of the Trust as well? You are. Yeah.
Vicky Barsby: Like again, with Neil's team being the guinea pig, we definitely use the lessons that we've learned from introducing the audits into, to Neil's team and to other teams across the Trust, and especially with the effective documentation review. The UTCs were early in the game to sort of get on board with that. So yes, there were definitely the ones that we learned from as a team. And the example that we show to other teams as well, we always say the UTCs have done this, and because of that, they've done this. It's yeah, we there are our poster child of the of the audits on AMaT.
Neil Jones: Speaking of posters, I think that's one of the things that we did from lessons learned from previous ones when EDR was launched to try and get it out there to all the staff, we had some brilliant posters made up, and me being me, I was putting them in the staff toilets and things so that people could not get away from seeing what was coming … captive.
Vicky Barsby: Audience? Absolutely.
Neil Jones: Well, they stood there washing their hands, you know, that's what they're looking at.
Dom Conlon: Oh that's fantastic. So anything else you'd like to kind of like cover, or sort of brag about and celebrate? Because it sounds like an amazing project. It really does. I mean, I was saying before we started this to Neil about the poster that led to, to me asking you to do this episode was just fascinating that the processes that you underwent. And it's only.
Vicky Barsby: When I think we have the opportunity to do things like the posters for the clinical audit conference last year that we actually stop and look back and reflect on what we've done in the journey that we've come from and sort of going from, like Neil says, paper based in a filing cabinet, collecting dust to actually one system that everyone can access and has that visibility across the Trust. It's when you step back and sort of go, wow, we did a lot. It's humbling sometimes and it's definitely worth celebrating. Like I say.
Dom Conlon: It really is. I mean, you mentioned before about telling people this is the result of your audit. This is what the benefit is. You've got to remember to do that for yourselves. So this is the benefit of the bigger picture. You know, we've got to do this kind of thing. So it sounds an amazing journey that you've all been on and, and shared with me today. So I'd just like to thank you very much for coming on. If anybody is wanting to, to celebrate any part of their job within audit and quality improvement and all that kind of thing, then please get in touch with me, podcast@amazon.co.uk and subscribe and share this episode wherever you can. And keep doing amazing work. So thank you very much.
Dom Conlon: Thank you, thank you, thank you.
The opportunities for data triangulation
Suzanne: Hello and welcome to the Clinical Audit and Improvement podcast from AMaT. The audit, management and tracking tool, which is developed in partnership with our users. My name is Suzanne Henderson, and in this episode we're going to be talking about the benefits of triangulation. With me today to discuss the subject are two guests. Welcome.
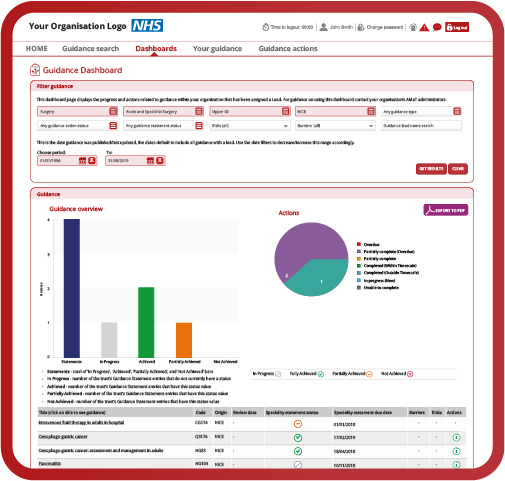
First to Mahdia Raheem Rasool, Madhi is the deputy head of clinical effectiveness at Birmingham and Solihull Mental Health NHS Foundation Trust. She has worked in both acute and mental health NHS Trusts, as well as in a private forensic mental health organisation. Her experience in clinical effectiveness has required her to oversee Trust-wide clinical audit planners, support senior directors with strategic work and support the review of NICE guidelines. She has a passion for supporting frontline staff, to ensure they are engaged and supported with clinical effectiveness and clinical and quality improvement.
And welcome also to Angela Ward, who joins us for the second time. Angela is a clinical audit and nice lead at Oxford Health NHS Foundation Trust. She's worked in both acute and community NHS Trusts, and has helped engage staff with using clinical audit for quality improvement. She's coordinated local audit plans, managed national project participation, promoted audit for accreditation and managed NICE compliance evidence. So we have a lot of experience on the podcast today. Thank you so much for joining. Maddie, so data triangulation, how does that play a part in your role currently?
Maddy: Hi Suzanne, firstly, thanks for having me on the podcast. It's a pleasure to be here.
I think data triangulation plays a big role in my role in clinical effectiveness, mainly because there's lots of data that we collect in health care on a daily basis. And I think it promotes that together, working. So bringing together different sources of data to support outcomes helps us to sort of. So one example will be the triangulation of clinical audit data with our risks and incidents. So it helps us to support our risks. So if we've got risks or risk registers in our Trusts, it helps us to sort of the audit data, can help us to support those risks as to how high or low they are. I think that's one thing a lot of clinicians struggle with is a scoring to one clinician, a risk might seem really high and to another clinician it seems quite low. And that's a debate that often happens in health care. But clinical audit data and nice benchmarking and things like that supports those scores and sort of gives it an evidence base. And obviously audits based on evidence. But also again, my first point being about that sort of together working it brings together, those data sources and those teams, to help them work more collaboratively. And I think that's when we work the best in health care, when we work collaboratively.
Suzanne: And when you're collecting that data, obviously it's coming from lots of different sources. Are they the sources that you're getting that data from? Are they engaged in this process of having that one aim? When you're looking at data triangulation, which is always really important, isn't it?
Maddy: Generally, I don't think they are. I think we could be better at having one aim and sort of when we're putting things on the risk register, that we can get better at looking what other data is out there. And when we're doing audits, looking at what we've already got on the risk register, what incidents are happening, and working together with these teams, I think we can be a lot better at that. I think it is improving with things like the PSIRF framework coming in that's, you know, the foundations of that on are on data triangulation. I'd be interested to hear what your view on that Angela.
Angela: Yeah, hi everyone. And thank you for having me back.
Yeah. I think PSIRF is going to be where we start to see data triangulation come into its own, because what it will do is it will help us guide well, help us see where we need to focus our resources on. So if we know the order, and complaints are saying there's an issue with a certain element of care, then our patient safety team could also look at monitoring incidents that fall under that same trend, things like that. So yeah, I do think that when it comes to PSIRF, data triangulation will be the way forward.
Suzanne: And it's having a, quite a robust process for triangulation, isn't it? Because they always say try not to take from too many sources. So having those three, four, potentially five different data points in it to get that big picture, and sometimes it's quite difficult to look at where that is. So if we take into consideration something like IPC. So let's look at the age old hand hygiene audit. And you look at that and the kind of data points that you're taking out from there to make sure that your assurance is okay. So let's have a look. You've got some high risks. So you've got something on the risk register around a certain type of infection, which, you know, you might get some clues with how are we doing on our hand hygiene audit. How are we doing on our estates audit? And also, you know, is staffing, do we get HR involved and do we get staffing rates in on that as well to see if we've got high turnover of staff? Is that something that you can openly have conversations with about what data you're triangulating to, to kind of achieve what you need to do to get that assurance?
Angela: Well, in a way, we are already sort of doing that in health care already, because if you look at our clinical governance structures, in our clinical governance meetings, they take data from a plethora of sources. And actually when they're reporting that each month they should already be looking at that data triangulation. This is something we need to get better at doing. But in a way we are already doing that. If you go down to a ward level or a service level, a manager should actually be looking at their data as a whole anyway, not just in pieces. So they should already be doing this in a way already.
Suzanne: Do you think they're looking at too much data sometimes? Because I think, you know, my experience of 16 years I was, which isn't actually as long as most people once you start talking to people. But, you know, sometimes they have this plethora of data in front of them. And it becomes become a bit of a minefield to kind of go, well, what's affecting what? And it's difficult, isn't it?
Maddy: Also the matter of sort of data accuracy as well. It's, I get the whole thing about there have been too much data, and sometimes we need to sort of hone in on the things that are a bit more relevant. And look at that bit. Folk have a like a focus piece looking at specific data, but there's also that data accuracy. Where are we getting this data from? Are the right people involved? Are we just looking at sort of Excel spreadsheets without having those conversations? I think it's really important to have the right people that are involved in that data, and putting it together, involved in the conversation needs to be, you know, a conversation rather than just looking at a data as one team, looking at somebody else's data. So I think data accuracy is a big thing as well as, you know, how much data you look at. Yeah. And a part of that is having the right people involved, the right stakeholders.
Suzanne: So if we take it right back and we have this, we look at data triangulation and we go, what does what does good triangulation look like? And what does non effective triangulation look like. You know where you're kind of a little bit lost and you don't really understand what all these measures are showing you. Do you have an example? Kind of or something in the past that you can go, that that worked really well, that you've learned from?
Angela: I suppose one that I've got and this is actually quite fairly recent. I'm looking at the Mental Health Act and how we comply with that at the moment, and our audit data and our Mental Health Act visit data show different things. So what we're going to be looking at is actually narrowing down our aim or focus and actually ask a specific question and look at the data that helps us answer that, rather than looking at all this data in isolation and trying to make it fit like two jigsaw puzzles coming together to make one. So I think it is bringing it right back down to is your question right at the start? Are you getting the data from the right places?
Suzanne: And there's for thinking about that sign up to safety initiative. They look at four different bits and data sources don't they. Where to get data from you know, their incident reporting, their admin data, case note review and point of care surveys. Is that kind of the four main bits that you would still get your data from. So, you know, if you look at your administration, administrative data, sorry, the HES data, the length of stay, readmission rates, staffing, things like that. Those are one, one bit of data, aren't they? They kind of get clumped together. And then you have those national audits, global trigger tools as well, which is your case note from your case note review kind of section. And I'm just wondering whether or not when we look at audit data, we don't use triangulation a lot. When we're looking at clinical audit in specifically on its own, we don't tend to go and now triangulate that data with other sources, do we, as part of the process or with assurance audits, really we tend to only be looking at it, I think, in the NHS from a risk point of view. And do you find that's still the case or is it, are people opening up now to data triangulation within clinical audit and improvement?
Angela: I think it's an area we need to be better at in audit. I think audit is the tool that people go to when they want to find out more data or say they want to do something. It's like saying, oh, we'll do a QR project on that. It used to be we'll do an audit on that, or it still is a bit, I know I promote looking at other sources of data, but I can say hand on heart, it's not happening regularly in the Trust I work in.
Suzanne: Birmingham and Solihull. When you're looking at audit results and you're doing the, so what is that? When you kind of move on to are there any risks? Is there any improvement? Where's the other data sources? Is that something that you're trying to do?
Maddy: We do, so I think we so ourselves a little different because our governance facilitators are within the Quality Improvement and Clinical Effectiveness team. So I think that's really, so we probably do it unconsciously sometimes. So when the governance facilitators are looking at like risk registers and things like that, they might if they're aware of audits going on, they might think, you know, well, maybe we need to link this data. But I think, as Angela said, I think we could definitely do a lot better. It's not something that we'd probably consciously do. But it is a lot more common, as in people are thinking about it a lot more. I went to an audit committee a couple of weeks ago, and they are at the bottom of their audit report. They had a section about risk, and the risk, how the audit outcomes linked to risk. So I think we've got the right set up to do it. We could probably get better at it. But the setup is there, and it possibly does happen unconsciously just because they're within the team and they don't know what's going on. And we sit with the Quality Improvement team as well. So that sort of merging and that flow of data of what's going on in Quality Improvement, how do we link that to audit? That's it's quite a natural data triangulation. But how that happens like sort of extended out of the team and things like that is probably something we need to get better at.
Suzanne: Yeah, I don't know. I don't know of any teams that routinely do it, yet from I guess as a so what as a follow on from a clinical audit project. So once you've got that baseline kind of going, you know we have these results. We're not doing too well in this area. Let's then have a look at everything at other areas, that tends to go through to key doesn't it? And at that point, I think naturally in quality improvement we collect data from multiple sources don't we? Whereas with the clinical audit, it's just the baseline that you're trying to get. How are we doing? How are we doing against this? Not kind of why aren't we.
Maddy: Sorry, I was just going to say I know when I work with Sheffield Teaching Hospitals, we used to routinely, I don't know if I can say this. Hopefully we do routinely risk assessed clinical audit outcomes. It was, there was a risk assessment form that was used for other risk assessments. Just part of the audit report.
Suzanne: I mean, we certainly are trying to get people to risk assess the project and the outcomes of the project or the results of the project. And I know working with Liverpool currently, they are very big on that as well. So I know that looking at risk and assurance levels is important, but it's more the how does that feed in. And it's really interesting that you brought up PSIRF earlier because, you know, we really want to help our organizations do that. And talking to the teams that we do serve is something that gets brought up constantly. And I think feeding in that audit data, feeding in that key data, feeding in the assurance audit data, feeding in your NICE guideline data, all against a theme just seems to be the perfect environment for real triangulation from those kind of, I guess, internal system measures that we've got. You know, external would be like your administrative stuff like HR and what have you.
Maddy: It just goes back to that conversation and I guess a piece of agenda, sort of with it being focused on sort of compassionate engagement and the systems based approach, it almost forces people to have those conversations about data triangulation and what's going on now, you know, in your area and sort of the incident data, what's going on in your area of, you know, quality improvement, clinical audit, things like that. I guess it brings together those people, rather than it being a sort of a bit of a blame culture, as the maybe the C framework was of, you know, we need to investigate this and find out what happened. It's more of a sort of a compassionate engagement. And we're getting together to really look at the nitty gritty details and bring the right information together.
Suzanne: What's interesting about that is if you're triangulating your data following an incident, I'm actually more interested in the so what moving forward because responding to the incident is fine, isn't it? And putting measures in place is fine. I would hate to think that that triangulation of data and the way that that was used in that response is then not continued. If it's been that beneficial, and I wonder whether or not if it doesn't exist already once people begin to look at the different sources, whether or not that becomes a permanent report within an organization and a permanent measure. I can just imagine SIRF beginning to really open up some avenues of learning that just haven't been there before.
Angela: In our Trust, we're starting to look more at dashboarding data from different sources. So we've got our own data warehouse and our own sort of like front end manipulation system. And the idea is eventually it will have this data warehouse, will have all the data coming from all our systems into it. So from this front end, we can then compare and contrast different areas, different systems, things like that. And that's a longer time project. But we're going to be doing a clinical effectiveness dashboard that will have data from various different sources. In a previous Trust I worked in, I did that under fundamental and better care. So pulling in HR data and complaints audit things like that. But also having a quality dashboard where you've got everything in one place, that makes it easier for people to see. But also some people don't know where this data is. They don't know we collect it. So actually having it in one place where people can click through it, or look through it, will make them think, oh, actually, I can look there for this data or oh, how does this compare to that? So I think dashboarding is going to be where you'll get more people on board with data triangulation.
Suzanne: That's music to my ears, because I've been saying for years when people are looking for systems and they're saying, does it pull in data from here? Does it pull in data from there? And very kindly, you have to kind of, you have to go but we shouldn't be pulling in data in this system. You should be using as fewer systems as possible, but you should be using the different systems within your organization. And then organizationally, you should be doing exactly that. You should have some sort of Quality Clinical Effectiveness dashboard that pulls in from everywhere. And that's where people go to view that activity. So do the activity elsewhere, but view it in that, in that, and not only that, if it's in your own business intelligence, you then get to change the dashboard as and when you need to, rather than waiting for the system to update to do that for you. So if you were going to buy a system that had that dashboard in capability, you'd have to be waiting a little while to make sure it could do the other things that you need to do, if you're controlling it within by your BI team will be able to do amazing things, especially if someone says, oh, we now need to report on that. Obviously you've got to get the capacity there, but they'll soon be able to build that in for you. And I think it's important when you're building systems to make sure that the output of that data is really simple, that they can just use those APIs or whatever it is, that they've got to get that data out and get it into your data warehousing. So I'm presuming you've got what Angela plans to put all your regular assurance audits in there. Your clinical audits.
Angela: Yes, so am I. That's got loads of APIs. So, the plan is we are going to pull the data from AMaT into our data warehouse. And then from there, because our front end is built in house we can then compare. Well, we can either view it in our data reporting system and then we can also link it to different data or compare and contrast to different data. So it's going to be a work in progress. We haven't started yet because we've had to change some clinical systems. But that is something that I will be back on my radar to do into, later 2024. But in the meantime, it's going to be very Excel dashboard, at the moment for.
Suzanne: Well, back old school, old school control of it, I love it, I love I love an Excel sheet. Oh that's fantastic. Maybe we can put you in touch with some people that we know are doing it as well. And a little bit further down the road on that. But no, that's fantastic. So when, going back to triangulation, what are you doing about your qualitative data? How are you getting that into kind of projects where you're having to display triangulated data? Lots of data.
Maddy: It's about getting it in the right forums and having it in the right forum as to where those people are that you triangulate it. So having sort of your clinical effectiveness, your patient safety, your risk teams all in the same forums and that qualitative data that you discussing, and then you've got that sort of evidence back up in like your minutes of meetings and things like that. And it goes back to like having the right people in the right room, I guess, with qualitative data.
Suzanne: Yes. It's difficult, isn't it? Because if you've got this, if you've got a mass of feedback and it's all in text form, it's very difficult isn't it, sometimes to, it's almost a project in itself because when you're looking at patient feedback or staff feedback, it's great with the more quantitative stuff. So are you happy with this? Yes. No. On a scale of 1 to 10, you know, you can look at that. But when you're looking at your comments, do you ever put that more free text based data into this kind of triangulation model, or do you tend to shy away from it a little bit?
Angela: I think most places will tend to shy away from it. The closest I've seen is us doing sort of like a trend analysis of comments or feedback or any other context put in, which is a start. And it's great, but it is something we could do better at it. I think sometimes people are afraid of it because they're more likely to do a, to have done a quantitative style analysis rather than a qualitative style analysis. So if you've never done that sort of analysis before, it is scary. And there's not a lot of help out there in most Trusts to do it as well. So I think that's something we do need to get better at. But we need to upskill people to do it. And I know myself it's one of my weakest areas and it's something I need to upskill with.
Suzanne: It's very time consuming as well, massively time consuming. So it doesn't surprise me that it's not something people readily embark upon. Talking about something taking a lot of time to do. Do you find that people, when they're wanting to see results and they're wanting to understand things, do you find you get pushback on going? Ah, but we need to look at these different sources because of the amount of time it takes. Or do you think the NHS now is going. No, we absolutely do need to triangulate data and look at it and then discuss it once we've got that. What are your pressures like at the moment.
Angela: Of the NHS at the moment, everything's time pressured. We're all short staffed and a bit frazzled and we could do with about doubling our staff and doubling our time. But you are always going to have the people that want the headline data ASAP, and then you're going to have the people who want the proper data in full later on. So it's about balancing some data you can triangulate quite quickly. Other data. It is going to take time, otherwise you lose the data quality with that. So actually if they want it next week and it's going to take a month to do the proper analysis, actually push back and say, do you want it done, rushed and potentially wrong, or do you want it done right? And you know, you're very sorry. You know, the data is completely accurate and you're always going to get better results from accurate data. Better from it, better anything from it.
Suzanne: What are your red flags? I mean, it's quite easy to see something that looks good isn't it? And it's quite often great to see something that really looks bad. But, um, is there anything that when you're looking at these different measures that kind of raises immediately raises any red flags for you currently?
Angela: Well, I'm quite sad. I tend to look at data in depth, so it's, I don't look at highlight data. I go into the detail. And so data quality is normally a red flag where things don't match up even along the same data set. So like responses to one questioner don't match how it should be in another one. So I tend to, those tend to be my red flags. Have people done their data quality right. And because I do look at it in that detail because I'm sad like that, I tend to pick that up and that's my red flag. I don't know if Maddie's got a different approach.
Maddy: I'd agree. I think that's quite a red flag, the data quality stuff. But I think, how people do it and methodologies and, you know, again, what sources they brought in and where they've taken from is one thing that I quite like to look at. And having that, going back to something you saying earlier that education and people, you know, do they know how to do things. Have we, if they're coming in and asking for sort of quick data or things like that, is it because they're not aware of the process and how long it takes? So I think the sort of the methodology and the way people do things is something that's quite important to me. And finding out why, you know, they're doing it in specific ways.
Suzanne: And are your teams trained? Are they? Data analysts first because without having. Yeah, I think that's the first question, isn't it? Because if you're looking at data integrity and quality and making sure there's no bias in any kind of data collection, are they are they trained in that or is it something? Because I know in most organizations I know there's very few that are actually trained in it. They tend to have learnt on the job, which again is a form of training, but I haven't had any formal training in data analysis.
Angela: Yeah, I think in my experience most people have learnt on the job or they do the basic Excel course or advanced Excel course and then do the data manipulation through that. I've had training, I've got a qualifications in data analysis, so but it isn't something we routinely train on. And I've had members of my team shadow the business information informatics team and things like that before to try and give them a little bit more of a understanding.
Suzanne: It's eye opening that, isn't it?
Angela: It is. But surprisingly enough, most people think they know it already. And then they do get that eye awakening opening. Yeah, yeah.
Suzanne: So Maddie mentioned methodologies. I don't think it's, you know, if you were to ask a lot of people looking at data now, you know, what's the methodology for that. Um, or which methodology have you applied. Because a lot of people come up with blank, don't they? And it's like, well, I just analyze the data and that's it.
Maddy: I guess it's a mix, I think in our in our Trust, it's good that our governance is in the data is working sort of audit and NICE and effectiveness because they have got that sort of, because they're looking at data all the time. They have got that experience with data and data analysis and stuff. I mean, I personally I'm just completing my PhD, so data and data analysis was a whole thing in first year. I had to learn a lot of data analysis very quickly. Yeah.
Suzanne: Because other people doing that will have, might have come from that background.
Maddy: Yeah.
Suzanne: That's a lot to learn.
Maddy: So yeah, there was a lot of data analysis involved in sort of the first year of the PhD, just how to do different methodologies and how to analyze different data, mostly qualitative, which was really insightful because a lot of my experience has been with quantitative.
Suzanne: Yeah. No, I do think that's really interesting. And also often in clinical audit you can get some really complex data data analysis and you, you know, you can spend ages on it. But the majority of clinical audits and assurance audits are pretty standard compliance based audits. Yes. No. Yes. No nays. Or, you know, you might have different weighted responses. And it's pretty basic stuff, isn't it? And as long as the question isn't biased, the question isn't, kind of it's clear and it's concise and it can't be seen in any other way. Those are pretty much your standards, aren't they? With regards to quality, do you do quality check when you're looking at data from audits and surveys, do you have someone that quality checks that before it comes through?
Angela: In theory, yes. In our Trust. But it depends who it goes through. So with audits, they should go through either my central team or through the governance team. So it really does depend on who you get I think.
Suzanne: And over the past say two three years or more I guess, have there been any cases that you can recall where data triangulation is really? Highlighted something that if you hadn't brought those extra data measures in, you just wouldn't have been able to see that bigger picture.
Angela: I think one for me is news, too. In one service, we were seeing more patient incidents relating to deterioration not being picked up. And yet the audits at the time were saying everything was hunky dory, which obviously the two don't match. But then patient feedback as well. We were seeing complaints. So yeah, that seeing those two, not those three not match prompted us to go in and look at it as a deeper dive and actually look at it more. I'm probably waffling now.
Suzanne: No, I love that because that's the whole point of it, isn't it? Yeah, it's the absolute whole point of it. It's nice to give you assurance, but so the other times it's almost like when you look at it, you look at these three, four, five points or whatever of data. And you, you know, let's take classic hand hygiene or any IPC related audit where everything's green. And then you go, you know, but we're still having this, you know, we're still having that. And everyone is trained up. You look at the training records, everyone is. So what's happening, you know, is it is it an environmental issue? And you really do start having to deep dive there. But at least you've got that information to hand. Maddie, if you were going to, if you were going to kind of say these are the things, what are your musts for triangulation? If you were going to if someone was starting afresh and they were in new into your role, what would your musts be?
Maddy: I'd say most things in clinical governance. So your risks, your incidents, your complaints, your legal things, stuff like that that you'd standardly take to sort of clinical governance meetings and have discussions about they're you're sort of standard agenda items.
Suzanne: And are there any issues with getting that data together currently? Do you find any challenges or is it all pretty to hand? And I think it.
Maddy: Goes back to the whole sort of knowing who's got the data, and knowing where it sits. It's all there with somebody, but sometimes people don't know the right people to go to. So it's about having those structures of which is where I think our in our organization, our facilitates, our governance facilitators are really quite handy because they've got their pockets in sort of governance, but they also sit within the effectiveness and the key team so they know what's going on there as well. So they're a great sort of central resource for us in our Trust. So I think it's about, you know, knowing who to go to, to where to get the data. And then that leads to sort of data accuracy, accuracy.
Suzanne: And would you change anything that you're currently doing if you had a big pot of money and all the time in the world, would you change anything?
Maddy: I think I would invest in a bigger audit team, but I'm guessing half the NHS Trusts in the UK would do that.
Suzanne: It's mental health and community Trusts for you. But yeah, you tend to have. They tend to be very much governance related. From my experience, they tend to have come from that role. But yeah, it is interesting seeing different structures. I mean, Angela, what did your role exist before?
Angela: Well, my current one. Yeah. Ish. It was merged with another role. Yeah. So yeah, my Trust is a prime example. I started off as a clinical audit and NICE guidance lead in a governance team in a directorate in this Trust. So and then they decided to invest more money in the Central Audit Team along with our merger into the Key Team. And my role came about I've actually doubled my staff in the last year and a bit because of it. So yeah, it is very weird how different Trusts have different setups and how some are very central centralized and how some are very arm's length.
Suzanne: And I don't think there are huge amounts of audit teams out there that have access to a lot of data that you would hope to, that you would hope they had access to, to be able to start looking at those triangulation points. But I don't know if that's because clinical audit will pass that on then, or if they do pass that on. So I don't know if they go this is the audit. This is the results. These are the actions we put in place. We're not looking anywhere else. That's not what a traditional clinical audit does. Do with it what you will, you know, maybe go on to do a key project. I don't think they have access readily to all the risks and incidents and complaints and those large governance reports, even if they get them, there might be like a little bit at the end going clinical audit. I don't think it's well embedded within it. And I think that's one of the things that PSIRF will do. Is that your experience as well, Maddie, with your audit profile, those junior doctor audits, you know, just the little very traditional clinical audits, do you find that they're they are accessible enough within the other governance and reports that you put out there?
Maddy: Yes and no. I guess it depends. I think if there's sort of directorates and the local areas are engaged in, in doing audits and QE and things like that. Yes. But then if they if they've got their own especially they've got their own sort of local audit committees and things, I think definitely yes. Because you have, you tend to have sort of like a multidisciplinary team in those committees. And I think having local audit committees is quite helpful for those kind of things. But if they've not got those, it's then it goes to sort of they go to governance, which is again like clinical governance meetings. It is accessible there because that's their core standard agenda items. Which is why, you know, I'll always go back to it, which is why I think it is quite good that our clinical governance facilitators are involved in audit. I mean, I'd love to get more of the time on audit, but that's another debate. You know, you could be getting yeah.
Suzanne: Getting governance teams that it is a difficult thing. You know, particularly in acute organizations. Traditionally that clinical old medical audit was so far away from the rest of governance, and nursing as well. And I think you do it better in community and mental health. I really do think you do. I think you have a better hold on the more being together. I think there's more of an overview, from my experience, anyway, from what I've seen. And then things are changing.
Maddy: Yeah, I think we do work a lot closer than I've worked with. When I worked in acute care, I think it was quite, they weren't distinctly quite separate, but they were sort of separate teams. And that, that sort of linkage was only when. So they used to risk assess clinical audit outcomes. That linkage was only when, oh, we've got a risk assessment I need to put it on your register. Can you do this? There wasn't that sort of that link for triangulation. Where? Here. As we work under one umbrella, it's more natural. So it doesn't seem it might not seem of these value sort of that that triangulation is happening. But it is it's just so natural that people almost don't see it, if that makes sense.
Suzanne: Yeah. And finally, the last thing I wanted to just touch on was the data itself and the challenges, I guess, of getting hold of the data, but more the format that people want data in now because as you know, we've moved over the last good five, ten years, the SPC charting and everything with process controls has been big. Is that something you've moved where appropriate to now? Do you have and do you have those skill sets for people to be able to understand them and read them correctly?
Angela: We're moving that way. I think our Trust has gone through quite a bit of change over the last few years, so we've had to change quite a few systems and how we're working, and we are going through a more embedded quality approach. So we are starting to move towards SPC and things like that with reporting data. That is something we are having to upskill a lot of people on, even on how to read it, let alone build it. But that is something I think every organization has gone through. We're all pretty much using the NHS England tools and templates and things, I know I am. So yeah, I think it's more just a case of it's a culture change that is slow in our organization, but it is happening. And I think the benefits of it, when people see the benefits, they are more on board with the change. So it's a slowly, slowly catchy monkey sort of like situation.
Suzanne: Yeah. Maddy, how are you getting along with? I think we're quite good.
Maddy: I think we've got quite an engaged community of people that see the benefit in sort of using SPC charts and, you know, tracking that data over time and the way that it's presented. Like there was a big thing around sort of the key team in introducing QR and the QR strategy and things like that and the branding and things, and that came with that. And I think as people got on board with that, they got on board with the benefits of how we present data better. Again, I agree with Angela. I think it's still a journey. But I think the Trust as a whole using they're better at presenting data than probably maybe five, six years ago.
Suzanne: Yeah. And do you find you get help and support and guidance nationally in relation to the data triangulation and sources and quality and what have you?
Maddy: Yeah, I think so. Again, it could be better. But what couldn't be better? It's a journey. I think that everybody's going on, that we just need to sort of persevere with and that understanding. But I think at the moment, the turnover of staff like sort of nationally, I guess in the NHS in general is a big thing. And it's like you educate one sort of team of people and it's great that, you know, they get on with it, they're doing things and then suddenly things change. So I guess it's adapting to change as well. But generally I think we do find the benefits of using sort of different tools and the way that we present things.
Suzanne: Well, here's to easier and clearer data triangulation in the future then. I think easier would be great, wouldn't it, where it's all just there and a push of a button that would. I think that's possibly the goal for everyone having nice, clean, robust data in front of them and being able to read it as well and act upon it because it's fine, isn't it? Getting all this data together, it's the it's the recording that you've done something about it and watching it change after that, isn't it? I guess we're all trying to get to.
Maddy: Not come back in the next couple of years and find the same thing, and then looking back and thinking, well, we did this a couple of years ago, you know, what happened? Where did we lose sight? So I guess it's about like, keeping that side of things as well.
Suzanne: Fantastic. Well, sadly, that's all we have time for today. Again, as always, there's so much to take away from it. And I know I definitely will with regards to the teams that we talk to and what have you. So thank you very much, both of you.
If any listeners would like to join us on a future episode, then email podcast@amazon.co.uk. This is a platform for anyone involved in clinical audit, to come and talk about the things that interest you and that can be outside of clinical audit as well. So improvement and assurance, you're all welcome as ever. Please subscribe and share wherever you can. Thank you very much for listening, and thank you very much to Maddie and Angela for joining us today.
How a QI project led to improved patient support after a diagnosis of bladder cancer
Dom Conlon: So hello and welcome to the Clinical Audit and Improvement Podcast from the audit, management and tracking tool developed in partnership with our users. My name is Dom Conlon, and in this episode I'm going to be learning about improving patient support after a diagnosis of bladder cancer.
Today's guests are all from East Kent Hospitals University NHS Foundation Trust. I have with me Pallab Kumar Sarkar, who's a urology registrar based in Kent and Canterbury Hospital, as is his colleague Rustam Karanjia. I've also got with me Hannah Waugh, who's a medical secretary in urology with a background in hospice and palliative care and as a special relevance to this episode, I'm also going to mention that once a week, Hannah does a shift at pilgrims, where she supports patients and their families going through terminal illness. So welcome to every one of you and thank you for joining me today.
Now, recent episodes of focused on various urology issues, and each one of them has shown how audit and quality improvement make a difference to improve patient outcomes and the patient experience. It strikes me from doing this and learning with all of you includes is really central to everything in health care. So I think, Hannah, it's only right that we begin with you. Your experience with bladder cancer is really personal. I wonder whether you'd mind telling us all about it, please.
Hannah: Of course. So, hi, everyone. I'm Hannah. I am unfortunately, have a very close connection to bladder cancer. Never thought I would, but it is the way it is. In May this year, my dad got diagnosed with stage three muscle invasive bladder cancer. Again, like I've said, it's a really surreal situation because you don't believe what's going on and how it's happening. So just to give a bit of background, my dad basically had two episodes of visible Hematuria in his urine. Both episodes were after having gone for a run and he the first time he had it, he didn't really think anything of it. And then when it happened again two days later, he thought, oh, something's not right here. So bless him. He went to the GP and got a couple of urine samples done, and they noticed that there was actually a lot of blood that was non visible in his urine samples. So they sent him on the two week wait pathway to Bournemouth Hospital where they both, where both my mum and dad live. They live in Bournemouth and so that's their local NHS trust. And within two weeks and I'm saying within two weeks because they've just been absolutely excellent.
They've made sure that, you know, everything's followed through as it should do. And he was given a flexible cystoscopy where he came face to face with the demon, which is the tumour, and it was 6 to 7cm with a couple of other tumours that were classed as lesions. I don't think they'd grown quite into tumours yet, but they'd obviously wanted to make sure that they were being monitored as well. So after his flexi, he was basically told that he'd need to have a Bty to have the tumours removed. Obviously we thought once he had that done that would be the, you know, the tumours gone and that could be possibly the end of the process. How wrong we were. You know, he had the Bty and was told that they couldn't actually remove much of the tumour because of how firm it was, and it had basically caused quite a lot of damage to the muscle side of his bladder. But it's weird because he never had really any symptoms, never had any pain, and yeah, basically just.
Rustam: Interject just for our listeners, what is a Bty.
Hannah: So it is an operation to basically go into the bladder to try and remove a sample of the tumour, to be able to be sent off for biopsy. Um, I think a lot of people have them done. I'm not sure on the process as such, because obviously I'm just talking from my dad's point of view, and there are a couple of consultants that I work for here at Kent and Canterbury. They don't actually specialize in bladder cancer as such. So it is something that I'm still coming to terms with and learning what it's all about really, but it is just a procedure to basically look into the bladder to remove a sample of the tumour, to basically either cure someone if the tumour is not that big, or to basically take a portion of it away to then send off so that they can obviously look at the histology behind what the tumour is. So basically the short answer is that dad was basically on the 4th of May, was diagnosed with grade three stage three muscle invasive bladder cancer and was told that he would be starting chemotherapy within a couple of weeks, which again, that was straight away how it worked. We were given the opportunity to basically go into his oncology appointments with him. And it was all really surreal.
I found it very, very upsetting and mean from a medical secretary's perspective. Obviously, I'm talking to patients all the time, but and from the hospice side of things. But when it's your own family member, my gosh, you don't realize how much it will affect you. And I found it personally really, really difficult. I was very, very distraught. I ended up having to actually leave the meeting because I just could not compose myself. And I think when my dad's sitting there being told his diagnosis, you don't really want somebody snivelling in the corner, no matter whether they're your daughter or not. So for me, it was about leaving and giving my mum and dad that opportunity to kind of be told the news, and then later on, they took me into a private room and had that conversation with me. And I've never experienced such brilliant. I mean, again, you don't really ever think you're going to have to experience a conversation about your loved one having cancer, but unfortunately, it probably will happen to all of us at some point in our lifetime. You know, 1 in 2 people are diagnosed with cancer, and that's a scary statistic. But, you know, for me, the excellent service, the ability that my dad has just finished chemotherapy and that's one that's one part of the journey ticked off.
And now we're going on to him. He's had a Pet scan. And they've basically said that there's no sign of the cancer metastasizing. So there's no spread for anybody who kind of wants the medical terminology in this. There's no spread. It has stayed within the bladder as much as it's muscle invasive. Obviously it's scary, but the chemotherapy is obviously kept the cancer from spreading at bay. And the next step is to basically flee. He's got an oncology appointment next week, and then we'll go from there. And I think he's got planned surgery for a cystectomy, which is a bladder removal at the end of September. So yeah, I mean, it's all very surreal. It's a huge roller coaster that we're all on. But I think my message to anybody is that you never think you're going to go through it. But at the end of the day, the way the medical world is at the moment and will continue to be there is so much support out there. And I think, you know, if you reach out and you get the right resources, it's something that you can come to terms with. I mean, I've had to learn that. So yeah, that's, that's, that's basically my part of this, you know, this question really. Thank you.
Dom Conlon: No thanks. No thanks for that. Hannah. Pallab, how common is bladder cancer in the UK?
Pallab: Hi I'm Pallab, one of the urology registrar working in East Kent University Hospital. Yeah. We are actually talking of about one of the most common cancer in the world. It's 10th most common cancer in the world. And if we take some statistics, if we take every 100,000 population, it happens in pretty much every nine person. So it's quite common. And it's very easy to get missed. That's why you should be a bit more proactive. As Hannah said in her dad's case, one spot of blood in the urine. And it's good that he went to see the GP. But still, there are a lot of a good number of population who sometimes ignore it, they think it could be. It's mainly because I think many of our patient population group is from an age where many times they feel like they can see all locations of blood in the urine and they ignore it. But yes, it is, as I said, it's a very common cancer and one of the most common urological cancer.
Dom Conlon: And how treatable is it, Rustam, do you want to kind of, like, talk about that, perhaps?
Rustam: Yeah. So it's, it really depends on everything, kind of what Hannah said as well. So I suppose the first from diagnosis, which is usually made with a camera test with the flexible cystoscopy when we look inside the bladder, after that, you can sort of gauge how big it is, if it has any components to it that look solid or looks like it's invading deeper inside the bladder. But really, the mainstay of treatment will be based on after the TURBT, which Hannah was mentioning before, which is, um, it stands for transurethral resection of bladder tumour. And it's a, it's a procedure where we look inside the batter with a kind of more rigid metal instrument, which is why patients are asleep. And what you're doing there at that time is you're scraping away the area that looks abnormal and just making sure it all goes. And what you're also trying to do is just you're trying to stage the tumour. And by that is by that I mean is it going into the muscle which is slightly deeper, or is it a more of what we call a superficial bladder cancer? And once you have those results in the lab and combined with the imaging that people have, so they usually have a CT scan that looks at the upper part of the kidneys as well, then you can make plans about treating the bladder cancer with various different ways.
Now, if it's more, more deeper into the muscle, which is in Hannah's father's experience, you may need more aggressive therapies such as radiotherapy or chemotherapy or even a cystectomy, but the more superficial ones can be treated with chemotherapies inside the bladder, or just simply with monitoring with camera tests at sequential points along the patient's journey. But I think that really the whole point about treatments that we've just heard from Hannah, I think really quite eloquently, is that it's not a bladder cancer, is not a one stop clinic. It's not a you see it, you get rid of it, that's it. You forget about it. It is a journey. And that everyone's journey will be slightly different. But it's that ongoing support that patients need going forward. I think that really impacts upon their journey for treatment of bladder cancer.
Dom Conlon: So that's interesting that you mentioned that kind of support there. And as Hannah mentioned about her own experience and having to step out of the room and letting her parents kind of discuss this as well and deal with it in theirs. This is going to I mean, this is and I know from personal experience that cancer in my family that this, this is a disease that absolutely can rock your, your life completely. How does it affect you? I mean, could you tell us perhaps about how it's affected you from just from day to day? As I say, as you said, your experience with this, you deal with this regularly. But from a personal point of view, it must have affected your life. And also, how has it affected your parents?
Hannah: Yeah, I think for me, you know, I thought I was prepared. You know, you always think that you're going to be, you know, prepared in any, in any sense because of the nature of what we do and the conversations I have on a daily basis with patients in the and in the hospice. But actually, when it's your own family, I guess it sounds really morbid, but the first thing you think of is, is this person going to die? Am I going to lose a loved one? and it sounds really naive because deep down, you know that actually, with the way medicine is nowadays, there's so many treatments out there that can be so effective at prolonging somebody's life. But in that moment, you kind of it kind of flashes before you and you think, God, life's really short. I mean, my dad's only 61 and he was, you know, it was just after his 61st birthday that he got diagnosed with this. And for someone so fit and healthy, I mean, he's a runner. He eats healthy. He doesn't really drink much. Maybe just a couple of glasses of wine at the weekend. You know, he was fit for his job because he was he basically is an engineer, so he's installing things. He's having to climb in and out of people's loft conversions and all that sort of stuff.
Hannah: So, you know, you look at life and you think actually, you know, you've got to enjoy it because you just never know what's around the corner. And for me, it rocked me in a way that I never realized it would. I mean, there's days where I really struggle and I still come to work because, you know, there's no good sitting at home and, you know, kind of drowning your sorrows that way. I actually find it incredibly rewarding coming to work, knowing that I'm talking to people who are probably going through a very similar experience to what my dad is at the moment, and actually being able to offer support. I mean, I'll have so many conversations with patients and I'll say, I completely get it. And when I say that, I say I actually do get it because this is my own experience on what I'm going through currently. And, you know, as soon as you say that to someone and you put yourself in that person's shoes and they then know that you're going through it, the connection that you have with people is very, actually very special. And I think you can offer so much support to people, you know, and, I mean, I've got a background in palliative care with the hospice. I've been working in the hospice environment, volunteering for five, nearly six years.
I lost both my grandparents were my dad's side within the hospice environment and the care and the, you know, the care, not just for the patient, but for the family was just incredible. But yeah, I just think it's a really hard one to describe. I mean, nobody knows what it's truly like for somebody going through it because it's somebody's personal journey and everybody deals with these things differently. And you find coping mechanisms, you find ways to come to terms with it in your own time. And there's days where I really struggle because they don't live near me. They're in Bournemouth. It's a good two and a half, three hours away. So I'm kind of spending my time in Kent and down there with them. But the knowing that I've got the care from here as well, the doctors, the consultants, everyone's just been exceptionally understanding and caring and it has made the experience a lot more easier in that, in that respect. So I feel very lucky as much as it's a horrible situation to be in. I do feel very, very lucky and actually very blessed to be in an environment when you're going through something like this because you're with like-minded people, people understand. So yeah, yeah.
Dom Conlon: I mean, obviously you've got a level of empathy there that is is greater than, than most of us will have. And I've got nurses in my family. But when it comes to the personal you turn to them. But they're also, you know, they become patients, they become relatives of patients and so on. So it does change that kind of thing. But obviously for the for the wider NHS and for, for your Trust in particular, the support system can't just rely on, you know, one secretary having gone through the experience or one nurse having gone through the experience or whatever. So what kind of systems are there to support you? What systems have you been able to draw upon down in Bournemouth that's helped all of your family? Yeah.
Hannah: So we're part of, luckily you know the way things are nowadays with social media. I did quite a lot of research into support groups, and we found a support group for Fight Bladder Cancer, which is a charity that was actually set up by somebody who was experiencing bladder cancer at the time and unfortunately has passed away now because of, you know, I think his was stage three, stage four muscle invasive. Again, it's very similar to my dad. So again, you know, when you're when you're looking at that, you think, my gosh. But think, you know, if this was a long time ago and since then you know medications, treatments, they've moved, they've moved forward with the times. Um, yeah. We're part of a support group where obviously a lot of people are putting posts up daily saying about their own personal journeys, their own experiences. And I found it found that very, very beneficial. And I actually got my dad into it. I mean, it took a while for my dad to come to terms with obviously the news. So he was very at the time he was very, you know, just wanted to kind of deal with it in his own way, especially being a man. Men deal with things differently. They're not as open. I'm very open as you can probably tell. And I had to kind of bring that openness out of him and say, look, there are so many ways that we can deal with this when you're ready. I mean, I always added when you're ready because you don't want to push somebody.
Everybody deals with things differently, and yeah, the support group has been really, really good. He's actually met a guy that lives down in Weymouth who's just about six weeks, eight weeks ago, had a cystectomy himself, and he's also a runner and he had exactly the same diagnosis as my dad, and has actually been given the all clear and will obviously be kept under surveillance, you know, think it's five years, obviously. And then you're basically classed as in remission. And I think that's still the way it works. Obviously, you know, you meet people who are going through similar experiences and until you know somebody else who's going through it, it's so beneficial for the patient because nobody else will understand. You know, you can say that you understand, but actually, deep down, you can only be there to kind of listen to what they feel and what they say. You can't personally think, okay, yeah, I completely get it because you're not the one going through it. So that's been really, really good. And I think things like that are so beneficial. Bringing people together, having like a group and a community of people who are going through similar diagnosis, it makes you feel like you're not alone because I think a lot of people will feel alone going through it. It's a very scary, traumatic, stressful, you know, it's a stressful time for people. And I think if you know other people going through it, it can help to carry you in your darkest moments with it.
So yeah, support groups, things like that. They're just so beneficial. And obviously a lot of them run through charities. So it relies on people doing fundraising. And I've actually, you know, will say it now, I've recently just raised over £3,000 for bladder cancer by doing I'm doing a 26 mile walk in a couple of weeks with my partner in London overnight. It's the shine walk and we're raising money for bladder cancer again and I think, you know, when you hear the stories from the charities saying you've, you've this money will enable so much more research, so much more ability to get patients seen quicker, the screening times for bladder cancer and the ability to obviously give people what they need during that really difficult time. I've turned it on its head really and kind of gone. Do you know what the way I'm going to cope with this is by helping other people? But that's just the way I am. I mean, that's why I enjoy work. I enjoy coming to work because I'm talking to people and I'm able to kind of go, do you know what? I get it. I understand. So yeah, for me, charity work's been a real big help during my experience with it because you just never know when you're going to need the help yourself. We never we never thought we were going to need it. And we do. So yeah.. Anything like that. Fantastic.
Dom Conlon: Yeah. Pallab. Awesome. I wonder if you could come at it from your, your perspective here.
Rustam: I think, Hannah, basically, I think it's really interesting to have heard Hannah's story over the last few weeks and months, just purely because we see it from such different perspective as clinicians. We see the patient or see the person. You know, maybe you should say for a few moments in their journey and you see them when you give them the diagnosis. You might see them after you've done the original tour, but you may see them in clinic, but you get such a small snapshot of what they're going through, and you often have to remember that. This is their moment of contact with you during their journey, and they really do. They obviously listen to everything you say very intently and hang off your every word. And it's all about the holistic side of number one. You need to be giving the right treatment and the right support and advice for them as well. But also it's about supporting them in that journey. And, listening to Hannah's experience in Bournemouth has really, I think, made Pallab and I both think about the support that we offer people here at East Kent, because it sounds like an excellent job has been done down there. And we do have some great resources here in East Kent with information. Our CNS team who aren't with us today are absolutely fantastic in managing patients in their ongoing care. But I think Pallab had a couple of ideas also about how we could increase the support that we have for patients here. And sorry, I'll let Pallab go.
Pallab: No, that's fine. Rustam you carry on.
Rustam: I was just going to say one thing I thought that I didn't know about even was the support Bladder Cancer UK that Hannah's been using online. And I think those online resources are really, really helpful. But just getting people together for their, you know, to see someone else who's going through the same thing that they are and also probably talk about some of the things that they don't want to talk about with us or they might find embarrassing or those other things is just probably extremely helpful. And, you know, many people deal with it in terms of families and relatives in different ways. And Hannah's been a real go getter when she's not laughing shrilly in the office, then, you know, she's out and about, raising money and doing so many different things. And that's her way of coping. And, you know, it's really amazing. But I'll hand over to Pallab, who's had a couple of thoughts about what else we can.
Dom Conlon: Fantastic.
Pallab: Thanks. To continue with what my colleague said, I actually didn't know about this online support group. I just came to know about the support group when we were talking about these podcasts. So regarding obviously Facebook support group or online support group, if we can't carry on or if we come to organisational support group in our trust, we got excellent CNS team. Because what I think or what I see for a patient when he comes to us in a room, we have a discussion. I believe the journey actually starts the moment they leave the consultation room, not when they come into the consultation room, because when they come to our room, they have a lot of expectation anxiety. They don't exactly know. And obviously I believe it's a human nature. They will always think something good will probably come up. It may not be the C-word or cancer, but by the time they come to room and we show them or we expect the news like, yes, you have most likely got cancer, I believe that's where the journey starts as a patient. And we do not spend that much time with them. Most of the time we are also stressed. We get 20 minutes, 25 minutes time. And in this time period we see them, examine them, break the news, give the plan and pretty much that's it. And after that, this patient may not see the same doctor again.
Pallab: The way the NHS is set up, he may not see the same doctor again. And in this small span of time period, we have to keep ourselves composed. We have to be sympathetic, we have to be empathetic, and we also have to be a clinician and doing all this stuff. Sometimes it's very easy to forget or not realise that this person sitting in front of me is not only a patient, he is a human too. So by the time he leaves the room, obviously I am sure many of the patients, their whole world is probably shattered because they just came to know that they've got cancer. Depending on the degree of severity. I'm sure even if we say like we don't know how long you are going to live or whether it is curative or not possible, they pretty much picture their whole life in front of them, their personal life, family, children, friends, social circle. I'm sure all this comes as a flashback in front of them. And then they go home. So that's where I believe we still need to improve.
There are a lot of steps or resources available in paper or in system, but in many times they don't translate into a practical scenario regarding their emotional well-being, social well-being. So in our hospital, I believe, and I can certify that we have got excellence who are actually specialist nurses. They usually try to fill the gap between the physician or urologist and the patient. They also have the clinical knowledge and they mix it up with the personal touch. And that I believe, would be really helpful. We have done this clinical forum for a few other cancers, especially prostate cancer, where we bring the patients for prostate cancer who are going to be operated and we bring all the patients together. One of our specialist nurses sit there. We pretty much give them a presentation of how their journey would be, what would be the operation or other treatment options, what could be possible complications, how you would feel, how our other patient felt, how they behaved. So we bring all those patients together. We give them a session of an hour or two. And obviously, as I said, there is a clinical nurse present. So that person can give answers to clinical questions, give answers to the person they need to call. When I was doing a bit of literature search, how or what other resources are available to improve the patient support, I found pretty much all the literature. They try to figure out the points where we can improve their social well-being, and it says it's mental support, social support.
And another interesting thing, I am not sure, I believe we don't talk about it that much, I actually came across this topic last year when I attended one of the conferences. Sexual health, which is rarely talked about in many of the literature, says many of the patients are really embarrassed when they start their journey in the first place. Because we are not talking about bladder cancer, we are talking about a very private part of a man or a woman. And I believe this gets ignored many times and many patients, according to the literature, said they feel embarrassed in the first place. Just thinking someone is going to look at their private parts or all the procedure that will involve manipulating those private parts. So these discussions, which probably doesn't make much sense to us as a doctor because we have been doing this every day. But as a patient who doesn't have much medical knowledge, these small things mean a lot to them.
But in our Trust, as I said, we have got this excellent support group from the CNS, but I believe we still can organise a social support group which can liaise with us. There should be a person of contact or key worker which already is in place in the NHS system, but it would be really nice if we can organise something in the community so that they can reach the person when they want.
Rustam: I think I'd just pick up on Pallab's point there as well, that it's just, as you say, just so many things people just don't have the confidence or feel empowered to speak to us, as healthcare professionals, about. And I think the other thing that those forums will do is just create something that, you know, Hannah and her dad have found so useful, which is that community, the sense of, you know, someone else going through it as well, and that companionship of that journey and, you know, having multiple people there. People will feel more empowered to talk about things that are maybe slightly personal to them, things about sex and, you know, ongoing function after surgery or after chemotherapy or after bladder installations that people may have as well. And I just think having a wider forum of people available will just really open up support groups and help people feel more, more happy with the journey that they're on.
Dom Conlon: Yeah, it sounds, I agree completely. So how do you begin to evaluate the effectiveness of all these systems? I mean, how do you even put them in in place at the Trust?
Pallab: So we can definitely start with the forum we are talking about. As I said, we already have been doing this for different other cancers, but we have not started or we have not thought about it for bladder cancer. And the way we can figure out the way we can do it is, we already know that number of patients on the list of patients who have been diagnosed with bladder cancer and is going to have some form of treatment or follow up. So, and again, we have got quite an effective system or efficient system to keep a track of all those patients. So we, we can bring the patients together.
Rustam: I think yeah, I think one of the interesting things is that we have those at the moment for patients who have typically, are going for radical prostatectomies. Now, the reasons that we do that is because having your prostate removed can really impact on patients continence issues and also erectile function as well, because the nerves run very close to the prostate. And really the benefit of those forums is that you educate men. You tell them what to expect, so they're less unhappy afterwards, but also warn them about pelvic floor exercises, the need for pads. You taking a medication like Viagra afterwards to help stimulate erections. And not only those, not only does that help in their recovery, but it also helps build expectations as well. Now, if we were to evaluate the progress of that, you could probably objectify it quite simply by looking at comparing people before and after the forum, looking at the number of pads they're using. If they do go to the forum or afterwards, say how much they leak, and erectile function as well. Now bladder cancer is a little bit more difficult because obviously we're not measuring functional outcomes. As such, we're really talking more about the symptom based things. So I think evaluation would probably be more subjective, as you would say. But you can formalise it a bit more with symptom based questionnaires. I suppose before and afterwards. That's something that we could do.
Dom Conlon: And the mental health side of it as well, I suppose definitely to measure that. Yeah. Hannah, I think you're probably going to be, you've probably got loads of ideas about how, from your own experience base about how you would improve the patient support. So what kind of, and I've no doubt that you're not shy about making your voice clear at your Trust either. So what suggestions have you put forward of your own?
Hannah: Well, I think at the end of the day, this is, it's something that needs to kind of be done because I think, you know, you want to try and stop the stigma. You want to try and give patients that, you know, that that understanding and knowing that, you know, they can come forward. So for me, you know, the support groups are really good, obviously on the outside, but we kind of need to have these running, running within the hospital environment. I know that the, I work with one of my other medical secretary colleagues, and we put together all the packs and things for the prostate cancer forum that runs every other week on a Thursday. And the amount of information and documentation that is given out to the patients, I think that gives people so much more understanding and takes away a lot of the worry and obviously the, the not knowing it. Like I said earlier, the not knowing is the worst part. And obviously, you know, going in for a big operation, you know, it's a big thing. You know, people don't like the thought of being put to sleep, going into general anaesthetic. And, you know, it's a scary process knowing that your life before the surgery and then coming out after surgery and the recovery time and the way that you have to come to terms with this new life. It's a big deal. So these support groups and these forums that are already running for other, you know, other cancers in the hospital, I think are very, very beneficial. And I think bladder cancer is takes up a huge percentage of all urological cancers alongside obviously your kidney cancers, your prostate cancers and things.
Hannah: There's so much more research into those and I think bladder cancer needs the same amount of resources and input. So yeah, maybe a forum that runs alongside the prostate forum, maybe every week that the prostate forum isn't running. There's one that's for the bladder cancer patients that offers understanding of chemotherapy, radiotherapy, even, you know, for the cancer patients that have got like the grade three, grade four, you know, going into the deeper element of bladder cancer. I think, you know, there should be a group that runs, that goes through all of the procedures that can be offered and the support. And I think for patients as well, knowing that they've got a key worker and someone that they can talk to. Having that contact and that, you know, building that sort of professional relationship with your doctor or your you know, your CNS is a huge thing because like the doctors have said, Rustam and Pallab, they, you know, it's a really personal journey and it's not something that you really want to open up to everybody about. I think, you know, talking to your doctor can be hard enough. The amount of patients I know that since, I mean, Run Park ran every week, for example, and there's been 3 or 4 people that have come over to me because where my bladder cancer vest for running and people have come over to me and gone, oh my gosh, my, you know, my husband or my uncle or my brother or they've been diagnosed with bladder cancer. What's kind of your story? And being able to kind of open up about it and raise awareness so that other people feel that they can go to the GP and get referred into hospital and get checked will help so many more people in the long term to not die from this awful disease. You know, there'll be so much more life quality and people will just be able to live life as normal as they can, whether they have to have, you know, life changing surgery such as a cystectomy. Because I think people also think, oh gosh, having a bag, that's really embarrassing. But actually, you know, it's a new way of life, but it's incredible that there is that option because I think my dad's my dad's take on it is that basically what's better to have a bag than to lose your life? Like he keeps saying to me, oh, I'll have this bag and it'll be like my bag of life. You know, he makes jokes about it, and he's got this. He wants to get this cover for his stoma bag, and it basically says nobody takes the piss better than me. It is really funny. And I think, you know, that's his way of dealing with it. And I think there's so many options out there. And if people were able to sit in a room and have that discussion with a cancer nurse specialist and, you know, have that opportunity to open up and speak about any concerns and questions they've got, it would just make life so much easier for a community of bladder cancer patients.
Dom Conlon: And talking about things is so important. I mean, like, I can just imagine you with the vest being a beacon for other people, it gives permission for other people to say, somebody I can talk to about this, somebody I can approach because it's out in the open.
Hannah: And definitely.
Dom Conlon: That's. Yeah, absolutely. Yeah. I think.
Pallab: Sorry for interruption, sorry.
Dom Conlon: Yeah.
Pallab: Obviously when a patient gets diagnosed and gets treatment, they know that they have to go through all these, all these fazes, which they may not probably would like to have, like a catheter or a bag or a scar. But he knows the support group. What they can do is help them to accept the fact, because at the end of the day, patient will accept it because most of the time, obviously most of the patient will prefer their life to not do anything, but the support group can help them to accept the fact in a more subtle way so that they don't feel that much stress, which can actually make them very mentally stressed.
Rustam: Yeah. And I think it's as you say, it's like it's validating it, isn't it? It's that someone else is going to go through it. Someone else has gone through it and they've been fine. And, you know, we can all talk about it. I mean, patients don't want to talk about things like that with Pallab or I mean, I think it's, and certainly not in the moments where they want, you know, their clinician to be there for them to talk to them about various other things because they are time limited. A lot of the interactions that we have patients and, you know, no one wants to open up to their doctor and talk to them about sex and all these other things as well. Well, at least not to me. I don't know, that's fine.
Pallab: It's the same with us. And it's not only the patient, and we also sometimes do not ask these questions as a clinician because when we diagnose a cancer, we become very focused on that cancer. Like we need to treat that. But obviously this diagnosis comes with collateral mental or emotional journey, which sometimes gets ignored.
Dom Conlon: And I suppose, as you as you both pointed out, when you're not always seeing the same patient, the same patient's not with you for their entire journey either. So it's a difficult thing to suddenly go, I'm going to put everything into you, and then I've got to repeat it all to the next.
Pallab: That's true. And when you see a patient again and again, you also develop that rapport. So your interaction becomes really different because still we see some patients who I mean, we see patients again and again who comes in clinic. And when you see a patient 1 or 2 times, next time when you see the patient, you can see the interaction is totally different. It's much more friendly. Patient is opening up with you and the discussion becomes really, the discussion becomes very precise. But both of you know that what you are talking about and he at that point, the patient actually points to you like, doctor, I really want you to sort this thing out. I don't have to look for problem. He will tell me, like, this is something bothering me. Can you please help me with this? But again, I think logistically it would not be possible for me, or for any clinician, to see the same patient again and again. But if there is a key person in between them, whether it's a formal key person in the setup or hospital setup, or informal key person in the community where they can open up, that makes their life much more easy.
Rustam: Yeah, I think the CNS often gets the real benefit of that, of that continued contact. Whereas yes, I would say it's more unusual for us at very occasionally you do get that follow up. I mean, consultants often do because they're under their name or care. But yes, it's less common for us, which is a shame. We'd love to see our patients again.
Dom Conlon: So I guess I've got I've got just two more questions really. But this all sounds a really straightforward, wonderfully straightforward path to improving patient outcomes. But there must be some obstacles to this. So I wonder if you could kind of outline a couple of them for me.
Pallab: Yeah. So the obstacles would be to set up the whole thing. First we need resources. Second, we need manpower. And third, we need coordination between resource and manpower and with the existing manpower. Obviously we all know that we are already stressed in NHS setup. It's very difficult to insert something new which would need more attention, but organizing a forum, I think we can do that. It doesn't need extra money, I believe from the health care support, what we need to make some space and if we can appoint one of our specialist nurses or similar person to coordinate between the patients to bring them, we can do that. Regarding, if we want to set up a community level key person formally, that would be quite challenging, frankly speaking, and that would need a really great push from higher up within our department. We can consider what we can, as I said, forum things from the patient perspective online support group. Those things are already there, so maybe we can help them to find out those social support groups. Because obviously many of the patients, in case of Hannah, she probably knows that. But imagine a patient who is at his 70s or 60s and who doesn't have that much access to internet or doesn't know how to use this internet. Obviously he doesn't know any of this, or she doesn't know any of this forum, so that person will be probably left alone. His journey would be between doctors, hospitals and the patient.
Rustam: I think one of the biggest barriers as well, following on from Pallab, is resource essentially. And the issue will be, I suspect going forward it's a time and money resource. Now, we could ask one of the team to see if they could do that, because they do that for the prostates at the moment. But our team, you know, they work unbelievably hard. I have to say they are completely filled to the rafters with clinics following up various other people. And so actually to get them to do an extra list will be very challenging. Although there is obvious benefits, the other option would be to create a new position or something else, or find a way to get funding for an extra person. But I think the difficulty with that would be, is that you, as we mentioned before, is that you want objective outcomes. How is this going to improve things? And as I said before, it's much easier with prostates because you can improve or show objective improvement and things like continence rates and erectile function, but more difficult for symptomatic and things that people would consider something maybe slightly softer, although that's probably not entirely true. And then I guess the final thing is that, you know, it's the NHS, and the NHS does trundle along relatively slowly. We do have lots of good ideas, and they do take a lot of traction to get off the ground. But I mean, as with all things in the NHS, fundamentally it is just a resource issue a lot of the time. So we'll have to make the business case for it, I suppose, and take things from there.
Hannah: I think as well, just quickly, I think as well, what would really help in these sorts of forums is having somebody who can offer a personal view on it. So like if, for example, there was somebody like myself, obviously, you know, my job is very busy. I am very, you know, I work for two really. You know, I work for Milan Thomas, who's a kidney surgeon, and he is the only kidney surgeon in our department. And I also work for Pejman Kheirandish, who does all the andrology side of urology, which is your erectile dysfunction. And patients who are struggling with fertility issues due to obviously, you know, problems with the erectile dysfunction area side of things. But I think I'd be happy to even offer my own services in a way, to kind of sit there and talk to these people and to kind of maybe have people that come in and actually offer their own experiences with it, because I think that would really, really help. But again, it's having the time and the resourcing to be able to do it.
Dom Conlon: Yeah. I mean, you've kind of, you've all kind of I think already answered this, but I usually end with if you could make one change what would it be? So let's, llet's go through Pallab. If you could make one change, what would it be?
Pallab: I would try to make the forum official. I would really try to do that.
Dom Conlon: Yeah. Rustam.
Rustam: I think if we're the forum would be fantastic. I think I would like an extra slot in between patients or just an extra ten minutes maybe for flexible after flexible cystoscopy to speak to patients and talk to them about everything that's going forward after their diagnosis. I just think that extra time just to talk to people would be great, but it essentially comes down to the same thing more resources and time to get that off the ground.
Dom Conlon: Of course.
Hannah: And Hannah again, you know, having gone through it in a personal stance, I think, you know, being able to offer my, my personal, you know, understanding towards other people. I mean, obviously, I speak to a lot of patients every day, and I do my very best to make every person's journey from a medical secretary side of things as easy as it can be. And I do struggle with the sense of, you know, there isn't always enough time in the day to give yourself to every single patient. But I think, you know, again, like Pallab, if we can get this forum lifted and going forward can have something running so that people can have that support and that understanding, I think it would just make, you know, the bladder cancer world within the NHS so much more beneficial and give people that, that support.
Dom Conlon: I've no doubt between the three of you that you've got the determination and the will to do it so I can see it being a success. Thanks very much for today. It's been absolutely wonderful and emotional as well, to be honest. That's all we've got time for. I'm going to let you all go now. And it's been it's been fantastic. But if anybody is listening out here who wants to join me on a future episode, then you can email podcast@co.uk. It's a platform for absolutely anybody involved to come and talk to me about the things that interest you and challenge you and how to, to lead to, to better patient outcomes. So please subscribe and share wherever you can. And thanks for much for listening.